
What is OCD
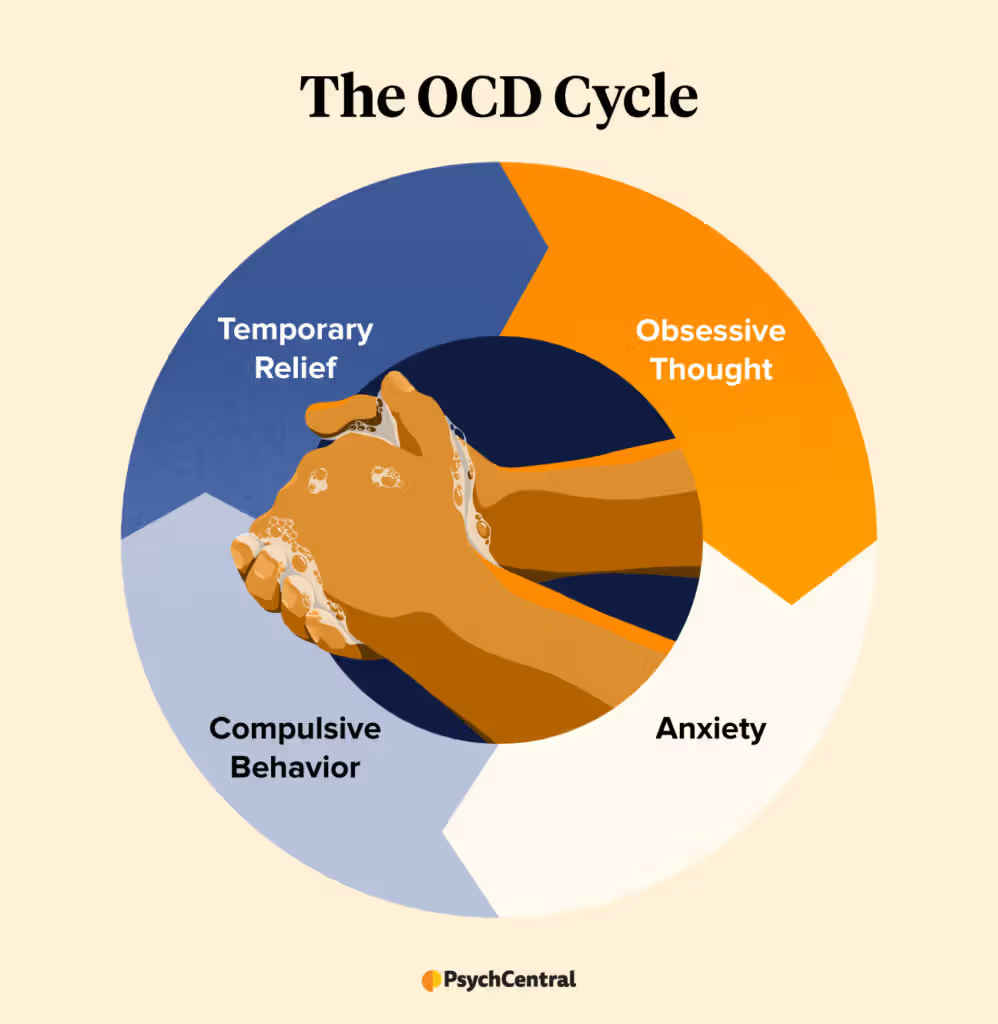
Long-term OCD is characterized by an individual’s inability to regulate recurrent, uncontrollable thoughts (called obsessions), compulsive activities (called compulsions), or both. OCD sufferers experience protracted symptoms that can be extremely upsetting or interfere with day-to-day activities. To help patients manage their symptoms and enhance their quality of life, therapy is available.
What are the signs and symptoms of OCD?
OCD sufferers may experience compulsions, obsessions, or both. Recurring thoughts, desires, or mental images that are bothersome, undesired, and cause anxiety in most individuals are called obsessions. Typical fixations consist of:
- Fear of germs or contamination
- Fear of forgetting, losing, or misplacing something
- Fear of losing control over one’s behavior
- Aggressive thoughts toward others or oneself
- Unwanted, forbidden, or taboo thoughts involving sex, religion, or harm
- Desire to have things symmetrical or in perfect order
Compulsions are recurring actions that someone feels compelled to perform, frequently as a result of an obsession. Typical compulsions consist of:
- Excessive cleaning or handwashing
- Ordering or arranging items in a particular, precise way
- Repeatedly checking things, such as that the door is locked or the oven is off
- Compulsive counting
- Praying or repeating words silently
signs and symptoms of OCD
Not every ritual or habit is a compulsion, and not every repeated idea is an obsession. On the other hand, OCD sufferers generally:
- Can’t control their obsessions or compulsions, even when they know they’re excessive.
- Spend more than 1 hour a day on their obsessions or compulsions.
- Don’t get pleasure from their compulsions but may feel temporary relief from their anxiety.
- Experience significant problems in daily life due to these thoughts or behaviors.
A tic disorder, which involves repeated motions or sounds, is also present in some OCD sufferers. Motor tics include abrupt, fleeting, repetitive movements of the eyes and other body parts,
such as grimacing the face, shrugging the shoulders, jerking the head or shoulder.
Sniffing, grunting, and frequent throat clearing are examples of vocal tics. Individuals diagnosed with anxiety disorders or mood disorders are frequently co-occurring with OCD.
Although they can appear at any time, OCD symptoms typically first appear in late childhood or early adulthood. Young adults are typically diagnosed with OCD.
OCD symptoms can appear gradually at first, then either subside or get worse with time.
The symptoms frequently worsen while under stress. Obsessions and compulsions can also evolve over time in an individual.
In order to cope, people with OCD may avoid circumstances that make them worse or turn to drugs or alcohol.
Many OCD-afflicted adults are aware that their obsessive habits are illogical.
Still, kids can not recognize that their actions are abnormal and frequently worry about horrible things happening if they don’t follow specific obsessive routines.
Children with OCD symptoms are usually recognized by their parents or teachers.
Speak with a healthcare professional if you believe that you or your kid may have OCD. OCD symptoms might worsen and interfere with everyday living if they are not treated.
What are the risk factors for OCD?

OCD is more likely to develop in those who have a number of risk factors, even though the underlying causes of the disorder are unknown.
Genetics: Research has indicated that an increased risk of acquiring OCD is linked to having a first-degree relative (parent or sibling) with the disorder.
Although no one gene or combination of genes has been proven to be the cause of OCD, research into the relationship between genetics and OCD is still being conducted.
Biology: Research on brain imaging has revealed that the frontal cortex and subcortical regions of the brain—regions that influence behavior regulation and emotional reactions—often exhibit abnormalities in individuals with OCD.
Additionally, researchers have discovered that a number of brain regions, brain networks, and biological mechanisms are important in the development of compulsive behaviors, obsessive thoughts, and the corresponding fear and anxiety.
To learn more about the relationship between specific brain regions and symptoms of OCD,
research is being conducted. This information can aid researchers in creating and modifying therapies that target particular areas of the brain.
Temperament: According to some research, those who grow up with more reserved habits, negative feelings, and signs of anxiety and despair are more prone to acquire OCD.
Childhood trauma: Studies have shown a link between symptoms of obsessive-compulsive disorder and childhood trauma. Further investigation is required to comprehend this correlation.
How is OCD treated?
Many people benefit from treatment, including those with the most severe forms of OCD. Psychotherapy, medicine, or a combination of therapies may be used by mental health practitioners to treat OCD.
A mental health professional can discuss the advantages and disadvantages of each treatment option and assist you in selecting the one that is best for you.
It’s critical to stick to your treatment plan because both medication and psychotherapy can take some time to start working.
While there isn’t a cure for OCD, there are therapies that can help sufferers control their symptoms, go about their daily lives, and lead fulfilled lives.
Psychotherapy
Psychotherapy is a useful treatment for OCD in both adults and children. Studies indicate that for many individuals, specific forms of psychotherapy, such as cognitive behavioral therapy and other associated therapies, can be just as beneficial as medicine.
For certain individuals, psychotherapy could work best in conjunction with medication.
Cognitive behavioral therapy (CBT) is a kind of talk therapy that aims to help patients identify false or damaging thought patterns so they can see and react to difficult situations more clearly.
Through CBT, individuals can learn to challenge these unfavorable ideas, assess how they affect their emotions and behavior, and alter self-defeating thought patterns.
CBT is often regarded as the “gold standard” of psychotherapy due to its extensive research.
The most effective use of CBT is when it is tailored to address the particular traits of particular mental illnesses, such as OCD.
Exposure and response prevention therapy (ERP): Studies have demonstrated that this particular form of cognitive behavioral therapy (CBT) successfully lowers obsessive behaviors, even in individuals who do not respond well to medication.
When using ERP, individuals spend time in a secure setting where they are progressively exposed to events that set off their fixation (like touching filthy objects) and keep them from performing their usual obsessive actions (like washing their hands).
Compulsions typically lessen as therapy progresses, despite the fact that this strategy may initially induce anxiety and increase the chance of early treatment termination.
Medication
Medication may be prescribed by medical professionals to treat OCD. Antidepressants that target serotonin, a chemical transmitter in the brain linked to OCD and depression, are the most often recommended drugs for OCD.
Among antidepressants, selective serotonin reuptake inhibitors are the most common class.
Antidepressant therapy for OCD may need greater doses than those used to treat depression, and it may take eight to twelve weeks for symptoms to start improving.
These drugs may have adverse effects on certain persons, like headaches, nausea, or trouble falling asleep.
The majority of OCD sufferers discover that taking medication can help them control their symptoms, frequently in conjunction with treatment.
The dosage of your medication might be changed over time by your healthcare professional to reduce adverse effects and withdrawal symptoms. Symptoms of Obsessive-Compulsive Disorder
Never stop taking your prescription without first consulting your physician. Together, you can monitor your health and safely and effectively modify your treatment strategy.
Other treatments
In 2018, the FDA approved the use of medicine, psychotherapy,
or a combination of both in conjunction with a deep form of repeated transcranial magnetic stimulation (rTMS) to treat individuals with severe OCD who did not respond to previous therapies.
This certification was expanded to include common TMS devices in 2022.
rTMS, a noninvasive therapy that uses a magnet to deliver repetitive low-intensity pulses to stimulate a specific area of the brain, is most frequently used to treat depression.
In contrast to conventional therapies, rTMS can specifically target brain regions linked to OCD.Symptoms of Obsessive-Compulsive Disorder
Deep brain stimulation (DBS) is a surgical technique that stimulates specific brain regions directly with electricity. When other treatments have failed,
medical professionals may utilize DBS to treat patients with severe OCD.
This treatment is regarded as experimental, nonetheless.
While DBS has been approved by the FDA to treat some neurological conditions, including Parkinson’s disease, its suitability for treating mental disorders is currently being investigated.
DBS has been authorized by the FDA for use as a Humanitarian Device Exemption in the treatment of severe OCD cases.
This exception permits the use of a medical device, like DBS, for uncommon diseases or ailments that impact a small number of patients,
making it difficult to compile sufficient data to prove the efficacy of the technology.Symptoms of Obsessive-Compulsive Disorder
The FDA website has the most recent guidelines and information regarding brain stimulation devices.
Finding Treatment
Call the Substance Abuse and Mental Health resources Administration (SAMHSA) Treatment Referral Helpline at 1-800-662-HELP (4357) for general information on mental health and to find treatment resources in your region.
Additionally, SAMHSA offers a location-based Behavioral Health Treatment Locator on their website. For further resources and information, go to the NIMH’s Help for Mental Illnesses page.
How can I find a clinical trial for OCD?
Clinical trials are investigations into novel approaches to illness and condition detection, prevention, or treatment.
Finding out if a novel test or therapy is safe and effective is the aim of clinical trials. Symptoms of Obsessive-Compulsive Disorder
Although taking part in a clinical study may benefit an individual, participants should understand that the main goal of a clinical trial is to obtain new scientific knowledge in order to better assist others in the future.
Numerous investigations involving patients and healthy volunteers are carried out by researchers at NIMH and across the nation.
Thanks to the discoveries made years ago by clinical trials, we now have more and better therapy alternatives. Participate in the medical advances of tomorrow.
See your doctor about clinical trials, their advantages and disadvantages, and if participating in one might be a good fit for you.
