1. Introduction to Schizophrenia

Definition of Schizophrenia
Schizophrenia is a severe and chronic mental disorder characterized by disturbances in thought, perception, emotions, and behavior.
It affects the way a person thinks, feels, and behaves, often impairing their ability to function in everyday life.
Symptoms of schizophrenia typically emerge in late adolescence or early adulthood and can persist throughout life.
Historical Perspectives
Schizophrenia has a complex history, with early descriptions of symptoms dating back centuries. Throughout history, individuals with symptoms resembling schizophrenia were often misunderstood and stigmatized.
It wasn’t until the late 19th and early 20th centuries that psychiatrists such as Emil Kraepelin and Eugen Bleuler began to describe and classify the disorder.
Their contributions laid the foundation for modern understanding and treatment of schizophrenia.
Prevalence and Incidence
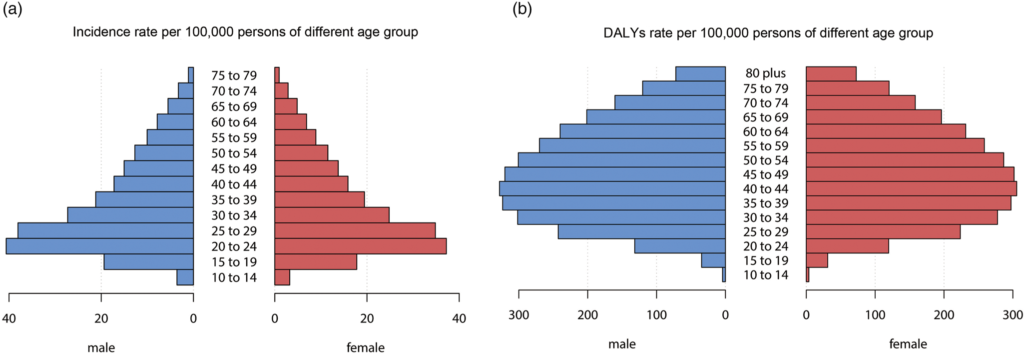
Schizophrenia affects approximately 1% of the global population, making it relatively common. However, the prevalence rates vary across different regions and populations.
Men and women are affected equally, but symptoms may manifest differently between genders. The onset of schizophrenia tends to occur earlier in men, while women may experience a later onset.
The disorder often results in significant personal, social, and economic burdens for individuals and their families.
2. Symptoms and Types of Schizophrenia
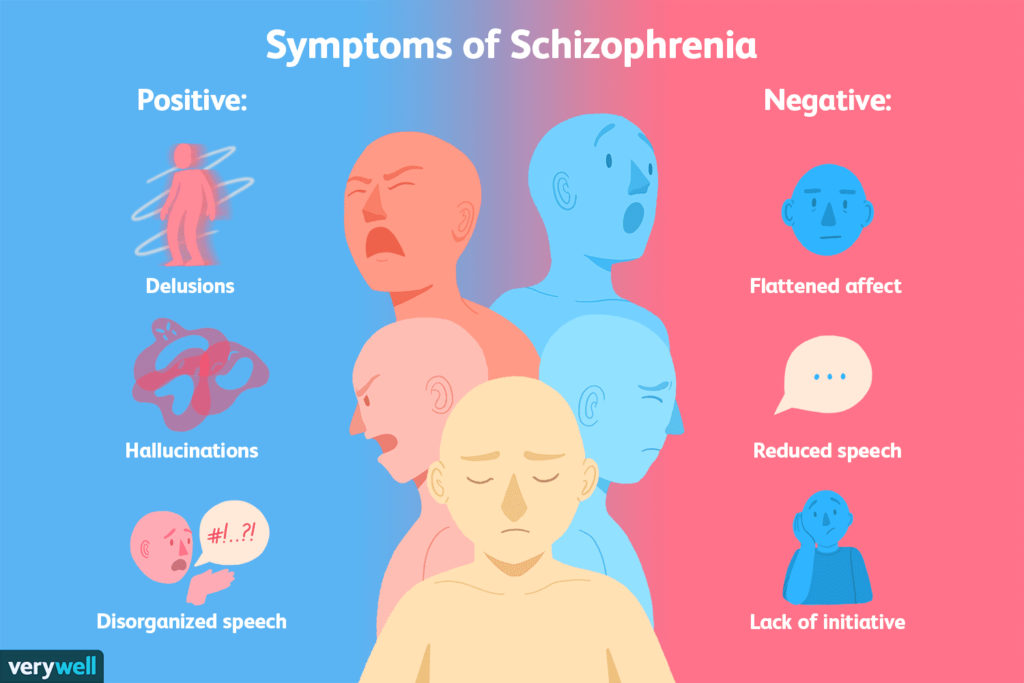
Positive Symptoms
Positive symptoms refer to experiences or behaviors that are added to a person’s normal repertoire of functioning. These symptoms often reflect an excess or distortion of normal functions.
- Hallucinations: Hallucinations are sensory perceptions that occur in the absence of external stimuli. Common types of hallucinations in schizophrenia include auditory hallucinations (hearing voices), visual hallucinations, olfactory hallucinations (smelling odors), gustatory hallucinations (tasting flavors), and tactile hallucinations (feeling sensations on the skin).
- Delusions: Delusions are false beliefs that are firmly held despite evidence to the contrary. In schizophrenia, delusions may take various forms, such as paranoid delusions (believing that others are plotting against oneself), grandiose delusions (believing one has special powers or abilities), or somatic delusions (believing that one’s body is diseased or altered).
- Thought Disorders: Thought disorders involve disturbances in the thought process, leading to disorganized thinking and communication. This may manifest as incoherent speech, tangentiality (derailing from the topic), or loose associations (jumping from one unrelated topic to another).
Negative Symptoms
Negative symptoms involve deficits or reductions in normal emotional, cognitive, or behavioral functioning.
- Affective Flattening: Affective flattening refers to a reduced range and intensity of emotional expression. Individuals with schizophrenia may exhibit blunted facial expressions, reduced vocal inflections, and a lack of emotional responsiveness.
- Alogia: Alogia, also known as poverty of speech, is characterized by a reduced fluency and productivity of speech. Individuals may provide brief or monosyllabic responses and may struggle to engage in meaningful conversation.
- Avolition: Avolition refers to a lack of motivation or interest in engaging in goal-directed activities. Individuals with avolition may have difficulty initiating and sustaining activities such as work, school, or personal hygiene.
Cognitive Symptoms
Cognitive symptoms involve impairments in various aspects of cognitive function, including attention, memory, and executive functioning.
- Impaired Attention: Individuals with schizophrenia may have difficulty focusing and maintaining attention, leading to distractibility and poor concentration.
- Impaired Memory: Memory deficits are common in schizophrenia, particularly in the areas of working memory and episodic memory.This can affect an individual’s ability to remember recent events, learn new information, and plan future actions.
- Impaired Executive Functioning: Executive functioning refers to a set of cognitive processes involved in goal-setting, planning, problem-solving, and self-monitoring. Individuals with schizophrenia may experience difficulties in these areas, leading to impairments in decision-making, organization, and social functioning.
3. Causes and Risk Factors

Genetic Factors
- Family History: Schizophrenia tends to run in families, indicating a genetic component to the disorder. Individuals who have a first-degree relative with schizophrenia have a higher risk of developing the disorder themselves.
- Gene Variants: Certain genetic variations and mutations have been associated with an increased susceptibility to schizophrenia. However, no single gene is responsible for the development of the disorder, and genetic factors interact with environmental influences.
Neurobiological Factors
- Brain Structure and Function: Studies using neuroimaging techniques have revealed structural and functional abnormalities in the brains of individuals with schizophrenia. These abnormalities often involve regions such as the prefrontal cortex, hippocampus, and thalamus, which are associated with cognitive function, emotion regulation, and sensory processing.
- Neurotransmitter Dysfunction: Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of schizophrenia. Excessive dopamine activity in certain brain circuits may contribute to positive symptoms, while glutamate abnormalities may affect cognitive functioning.
Environmental Factors
- Prenatal and Perinatal Factors: Adverse events during pregnancy and childbirth, such as maternal infections, prenatal malnutrition, maternal stress, and complications during delivery, have been linked to an increased risk of schizophrenia in offspring.
- Urban Environment: Growing up in urban environments has been associated with a higher risk of developing schizophrenia, possibly due to factors such as social stress, exposure to pollutants, and reduced social cohesion.
Developmental Factors
- Early Life Experiences: Childhood adversity, trauma, and social isolation are associated with an increased risk of developing schizophrenia later in life. Stressful life events during critical periods of neurodevelopment may contribute to the onset of the disorder.
- Neurodevelopmental Abnormalities: Disruptions in early brain development, including synaptic pruning, myelination, and neurotransmitter systems maturation, may predispose individuals to schizophrenia.
4. Diagnosis and Assessment
DSM-5 Criteria
- The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is the standard classification system used by mental health professionals for diagnosing psychiatric disorders, including schizophrenia.
- DSM-5 criteria for schizophrenia include the presence of characteristic symptoms (e.g., hallucinations, delusions, disorganized speech) lasting for a significant portion of time during a one-month period, with continuous signs of disturbance persisting for at least six months.
Clinical Assessment
- Clinical assessment of schizophrenia involves a comprehensive evaluation of the individual’s symptoms, medical history, family history, and psychosocial functioning.
- Mental health professionals may use standardized assessment tools, interviews, and observation to gather information about the nature and severity of symptoms, as well as the impact of the disorder on daily functioning.
Differential Diagnosis
- Differential diagnosis involves distinguishing schizophrenia from other psychiatric disorders and medical conditions that may present with similar symptoms.
- Conditions that may mimic schizophrenia include mood disorders (e.g., bipolar disorder), substance-induced psychotic disorders, schizoaffective disorder, delusional disorder, and psychotic symptoms associated with medical conditions or substance use.
- Differential diagnosis requires careful consideration of the temporal pattern of symptoms, the presence of mood disturbances, the course of illness, and response to treatment.
5. Treatment Approaches

Medication
- Antipsychotic Drugs: Antipsychotic medications are the primary treatment for managing symptoms of schizophrenia. These medications help to alleviate positive symptoms such as hallucinations and delusions by blocking dopamine receptors in the brain.
- Side Effects: Common side effects of antipsychotic drugs include weight gain, metabolic disturbances, extrapyramidal symptoms (e.g., tremors, stiffness), sedation, and sexual dysfunction. Newer atypical antipsychotics are associated with a lower risk of some side effects but may still cause metabolic and cardiovascular complications.
Psychosocial Interventions
- Cognitive Behavioral Therapy (CBT): CBT aims to help individuals with schizophrenia identify and challenge maladaptive beliefs and thought patterns, manage symptoms, and improve coping skills. CBT can be effective in reducing distress associated with hallucinations and delusions, improving medication adherence, and enhancing social functioning.
- Family Therapy: Family therapy involves educating family members about schizophrenia, improving communication and problem-solving skills, and reducing family stress. Family therapy can help improve family relationships, reduce caregiver burden, and enhance social support for individuals with schizophrenia.
- Social Skills Training: Social skills training programs teach individuals with schizophrenia interpersonal and communication skills, problem-solving strategies, and assertiveness techniques. These programs aim to improve social functioning, reduce social isolation, and enhance community integration.
- Supported Employment: Supported employment programs provide vocational training, job placement assistance, and ongoing support to help individuals with schizophrenia obtain and maintain competitive employment. These programs emphasize the importance of meaningful work, financial independence, and social inclusion in the recovery process.
6. Recovery and Management

Early Intervention Programs
- Early intervention programs aim to identify and treat schizophrenia in its early stages, often during the prodromal phase or following the first episode of psychosis. These programs provide comprehensive assessment, medication management, psychosocial interventions, and support services to promote recovery and prevent relapse.
Rehabilitation Programs
- Rehabilitation programs focus on helping individuals with schizophrenia develop the skills and confidence needed to live independently and participate fully in community life. These programs may include supported housing, life skills training, education and vocational support, and recreational activities tailored to individual interests and abilities.
Relapse Prevention Strategies
- Relapse prevention strategies involve identifying early warning signs of relapse, developing coping strategies, and implementing proactive measures to prevent symptom exacerbation and hospitalization. Strategies may include regular monitoring of symptoms, medication adherence, stress management techniques, and crisis planning.
Support Networks
- Support networks play a crucial role in the recovery and management of schizophrenia by providing emotional support, practical assistance, and social connections. Peer support groups, online forums, and community organizations can offer validation, encouragement, and opportunities for socialization and advocacy.
7. Living with Schizophrenia

Coping Strategies
- Psychoeducation: Learning about schizophrenia, its symptoms, and treatment options can empower individuals with the disorder and their families to better understand and manage the condition.
- Medication Adherence: Adhering to prescribed medication regimens is essential for managing symptoms and preventing relapse. Developing strategies to remember medication schedules and addressing concerns about side effects can help improve adherence.
- Stress Management: Stress can exacerbate symptoms of schizophrenia. Engaging in relaxation techniques such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can help reduce stress and promote emotional well-being.
Stigma and Discrimination
- Public Perception: Despite advances in understanding and treating schizophrenia, stigma and discrimination against individuals with the disorder persist. Misconceptions and negative stereotypes contribute to social exclusion, employment discrimination, and barriers to accessing healthcare and support services.
- Anti-Stigma Campaigns: Education and advocacy efforts aimed at challenging stereotypes, promoting empathy, and fostering inclusive communities are essential for reducing stigma and discrimination associated with schizophrenia. Anti-stigma campaigns, media representation, and storytelling initiatives can help raise awareness and promote social acceptance.
Advocacy and Support Groups
- Peer Support: Peer support groups provide opportunities for individuals with schizophrenia to connect with others who share similar experiences, challenges, and goals. Peer support can offer validation, encouragement, and practical advice for coping with symptoms, navigating treatment options, and accessing community resources.
- Advocacy Organizations: Advocacy organizations and mental health advocacy groups play a vital role in promoting the rights, dignity, and well-being of individuals with schizophrenia. These organizations advocate for policy reforms, funding for research and services, and initiatives to improve access to quality care and support.
8. Research and Future Directions

Advances in Neuroscience
- Neuroimaging Studies: Advances in neuroimaging techniques, such as functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI), have provided insights into the structural and functional abnormalities underlying schizophrenia. These studies help elucidate the neurobiological mechanisms of the disorder and identify potential targets for intervention.
Pharmacological Research
- Novel Treatment Approaches: Ongoing pharmacological research aims to develop new antipsychotic medications with improved efficacy and tolerability profiles. Research efforts also focus on targeting specific neurotransmitter systems implicated in schizophrenia, such as the glutamatergic and cannabinoid systems, to address cognitive and negative symptoms.
Psychosocial Interventions
- Personalized Treatment Strategies: Research on psychosocial interventions seeks to identify effective strategies for tailoring treatment to individual needs, preferences, and goals. Personalized approaches may include integrating technology-based interventions, enhancing family involvement, and addressing cultural and socioeconomic factors that impact treatment outcomes.
Genetic Studies
- Genomic Research: Genome-wide association studies (GWAS) and other genetic approaches have identified numerous genetic variants associated with schizophrenia. Integrating genetic data with clinical and neurobiological findings may help elucidate the complex etiology of schizophrenia and inform the development of targeted interventions.
9. Conclusion

Recap of Key Points
- Schizophrenia is a complex and debilitating mental disorder characterized by disturbances in thought, perception, emotions, and behavior.
- The disorder is associated with a combination of genetic, neurobiological, environmental, and developmental factors.
- Symptoms of schizophrenia include positive symptoms (e.g., hallucinations, delusions), negative symptoms (e.g., affective flattening, avolition), and cognitive symptoms (e.g., impaired attention, memory deficits).
- Diagnosis and assessment of schizophrenia involve careful evaluation of symptoms, medical history, and psychosocial functioning, guided by standardized criteria such as the DSM-5.
- Treatment approaches for schizophrenia include medication, psychosocial interventions, rehabilitation programs, and support networks tailored to individual needs and goals.
- Living with schizophrenia presents challenges related to coping with symptoms, managing stigma and discrimination, and accessing supportive resources and services.
- Ongoing research in neuroscience, pharmacology, psychosocial interventions, and genetics offers hope for advancing our understanding of schizophrenia and improving treatment outcomes.
Challenges and Opportunities
- Stigma and discrimination continue to pose significant barriers to effective treatment and community integration for individuals living with schizophrenia.
- Access to quality mental health care, including early intervention programs and evidence-based treatments, remains limited in many regions.
- Disparities in healthcare access and treatment outcomes highlight the need for targeted interventions and advocacy efforts to address systemic barriers and promote health equity.
- Opportunities for collaboration among researchers, clinicians, policymakers, advocacy organizations, and individuals with lived experience are essential for driving innovation and fostering positive change in mental health care.
Hope for the Future
- Advances in research, treatment, and public awareness offer hope for improved outcomes and quality of life for individuals living with schizophrenia.
- Emerging technologies, personalized treatment approaches, and holistic models of care hold promise for enhancing early detection, intervention, and recovery-oriented support.
- Continued efforts to reduce stigma, increase access to mental health services, and promote social inclusion can contribute to a more compassionate and supportive society for individuals affected by schizophrenia.
- With dedication, empathy, and collective action, we can work towards a future where all individuals living with schizophrenia receive the care, respect, and opportunities they deserve.
